
None of the trials of intensified anticoagulant therapy tested anticoagulation in combination with an antiplatelet agent.Īll analyses were done according to the intention-to-treat principle and included all patients from the time of randomisation. Meta-analysis of trials of intensified anticoagulant therapy showed a reduction in venous thromboembolism but no mortality benefit. These data raised the possibility that a longer course of treatment might be of benefit. However, in the three largest colchicine trials, one found no evidence of benefit with up to 10 days of colchicine treatment, and the other two suggested a benefit with 15 to 30 days of treatment. Meta-analyses of randomised trials indicated no overall benefit of colchicine in patients hospitalised with COVID-19.

We searched PubMed from Jan 1, 2020, to the present using the search terms, “anticoagulation OR anticoagulant OR thromboprophylaxis OR antithrombotic”, “heparin” OR UFH OR unfractionated-heparin OR LMWH OR “low molecular weight heparin” OR dalteparin OR enoxaparin OR NOAC OR DOAC OR “direct oral anticoagulant” OR “novel oral anticoagulant” OR “non-vitamin K antagonist oral anticoagulant” OR “apixaban” OR “rivaroxaban” OR “edoxaban” OR “dabigatran”, “coronavirus” OR “COVID” OR “coronavirus disease-2019” OR “coronavirus 2019” OR “COVID19” OR “covid-19”. No patients assigned to rivaroxaban and aspirin had serious adverse events that led to discontinuation of study drug. 17 (1♶%) patients assigned to the combination of rivaroxaban and aspirin had bleeding compared with seven (0♶6%) of those allocated to control (p=0♰42) the number of serious bleeding events was two (0♱9%) versus six (0♵7%), respectively (p=0♱8). Among patients assigned to colchicine, 8 (0♶1%) had adverse events that led to discontinuation of study drug, mostly gastrointestinal in nature. There was no increase in the number of patients who had at least one serious adverse event for colchicine versus control groups (87 of 1304 vs 90 of 1307) or with rivaroxaban and aspirin versus control groups (85 vs 91 ). Results were consistent in subgroups defined by vaccination status, disease severity at baseline, and timing of randomisation in relation to onset of symptoms. Overall, 368 (28♲%) of 1304 patients allocated to colchicine and 356 (27♲%) of 1307 allocated to control had a primary outcome (hazard ratio 1♰4, 95% CI 0♹0–1♲1, p=0♵8) and 281 (26♴%) of 1063 patients allocated to the combination of rivaroxaban and aspirin and 300 (28♴%) of 1056 allocated to control had a primary outcome (HR 0♹2, 95% CI 0♷8–1♰9, p=0♳2). 2611 patients were included in the analysis of colchicine (n=1304) versus control (n=1307) 2119 patients were included in the analysis of rivaroxaban and aspirin (n=1063) versus control (n=1056). Findingsīetween Oct 2, 2020, and Feb 10, 2022, at 62 sites in 11 countries, 2749 patients were randomly assigned to colchicine or control and the combination of rivaroxaban and aspirin or to the control.
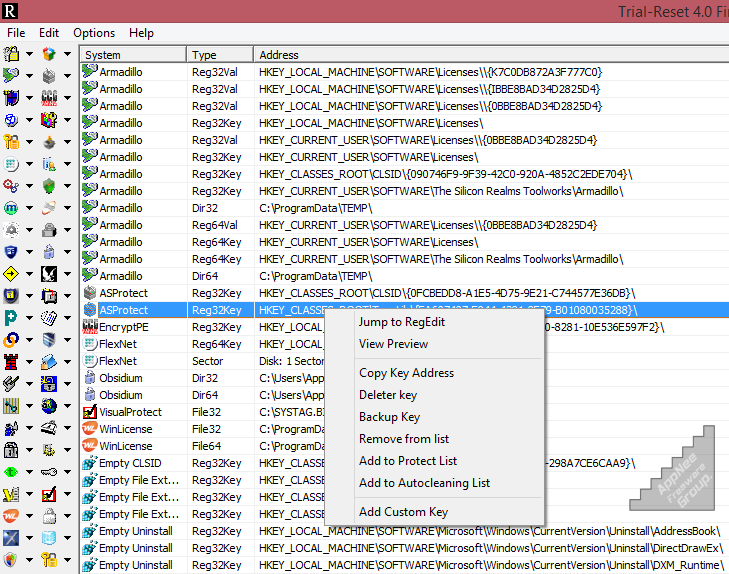
#Trial reset v4.0 final descargar trial#
The trial is registered at NCT04324463 and is ongoing.
#Trial reset v4.0 final descargar plus#
The primary outcome, assessed at 45 days in the intention-to-treat population, for the colchicine randomisation was the composite of the need for high-flow oxygen, mechanical ventilation, or death and for the rivaroxaban plus aspirin randomisation was the composite of major thrombosis (myocardial infarction, stroke, acute limb ischaemia, or pulmonary embolism), the need for high-flow oxygen, mechanical ventilation, or death. Investigators and patients were not masked to treatment allocation. Patients aged at least 18 years with symptomatic, laboratory confirmed COVID-19 who were within 72 h of hospitalisation or worsening clinically if already hospitalised were randomly assigned (1:1) to receive colchicine 1♲ mg followed by 0♶ mg 2 h later and then 0♶ mg twice daily for 28 days versus usual care and in a second (1:1) randomisation, to the combination of rivaroxaban 2♵ mg twice daily plus aspirin 100 mg once daily for 28 days versus usual care. The ACT inpatient, open-label, 2 × 2 factorial, randomised, controlled trial was done at 62 clinical centres in 11 countries. The Lancet Regional Health – Western Pacific.The Lancet Regional Health – Southeast Asia.The Lancet Gastroenterology & Hepatology.


 0 kommentar(er)
0 kommentar(er)
